IBS symptoms rarely come from one isolated issue. Digestion is part of a wider system that includes how your body handles energy demands, stress, recovery, sleep, and day-to-day load.
Food matters — but it’s only one input. Gut function is also influenced by how consistently your system can regulate itself under pressure. When that regulation is strained, digestion often becomes more reactive and less predictable.
In practice, this means symptoms may fluctuate:
even when diet stays the same
during periods of disrupted sleep or travel
under sustained work or training pressure
after illness or long-term restriction
This is why symptoms can appear inconsistent or hard to control with food alone.
Through experience, I’ve found that progress happens when digestion is assessed alongside the other systems that influence it, rather than treated as a stand-alone problem.
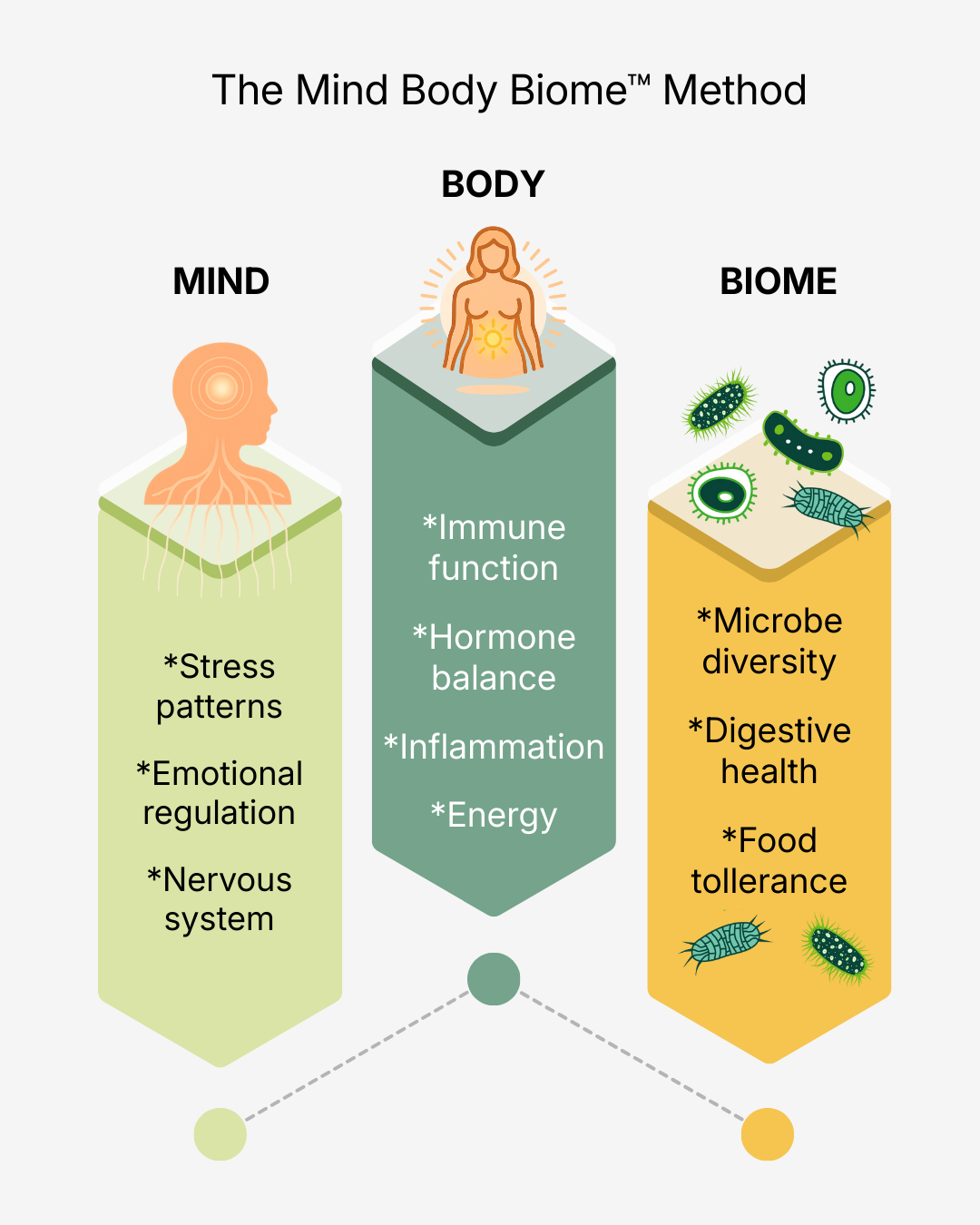
This approach looks at three interacting areas that influence gut function:
The gut and microbiome — digestion, absorption, and microbial balance
The body — energy availability, sleep, recovery, hormones, and load
The nervous system — how your system responds to ongoing pressure and stress
When these are considered together, patterns start to emerge. Symptoms that once felt random often begin to make sense, allowing changes to be made in a targeted, efficient way rather than through trial and error.
This framework provides structure to the process, so decisions are based on how your system is responding — not on guesswork or generic advice.