Q1: What is the difference between a gut health dietitian and a gut health nutritionist?
A: Many people search for a gut health dietitian or gut health nutritionist when looking for support with bloating, reflux or ongoing digestive symptoms. In the UK, "dietitian" is a legally protected title, while "nutritionist" and "nutritional therapist" are regulated through professional bodies such as BANT and CNHC. Dietitians typically work in medical settings and focus on clinical testing, diagnosis and medical nutrition interventions.
A gut health nutritionist takes a more holistic approach, using personalised nutrition, supplementation, lifestyle medicine and functional testing to address the root causes of digestive issues. As a registered Nutritionist and Nutritional Therapist (BANT, CNHC), my work combines these tools to support long-term gut health.
Q2: What is a gut health nutritionist, and how can they help with bloating or reflux?
A: A gut health nutritionist is a registered professional who specialises in digestive health. They support people with bloating, reflux, constipation and other gut symptoms by identifying food triggers, improving digestion and restoring microbiome balance.
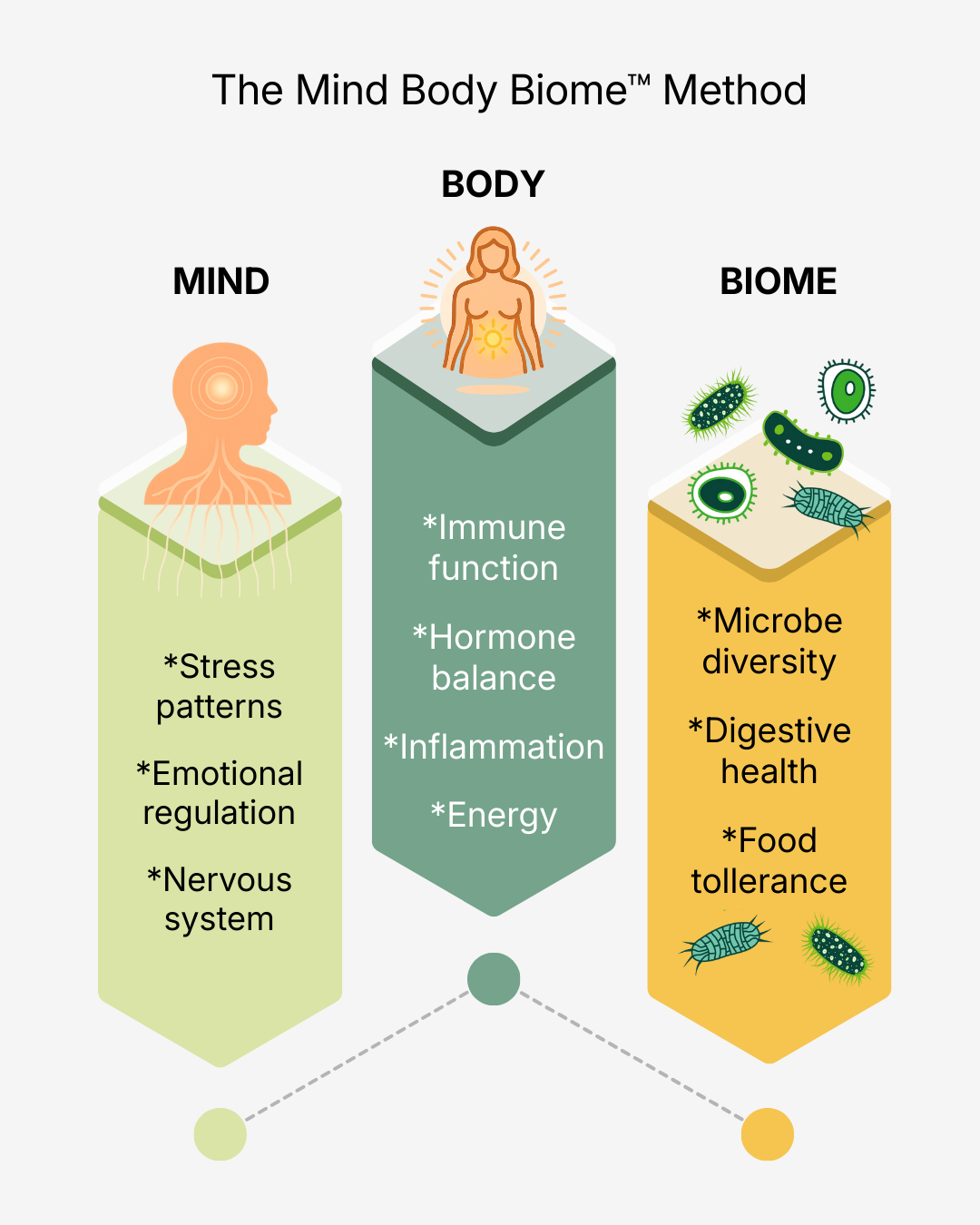
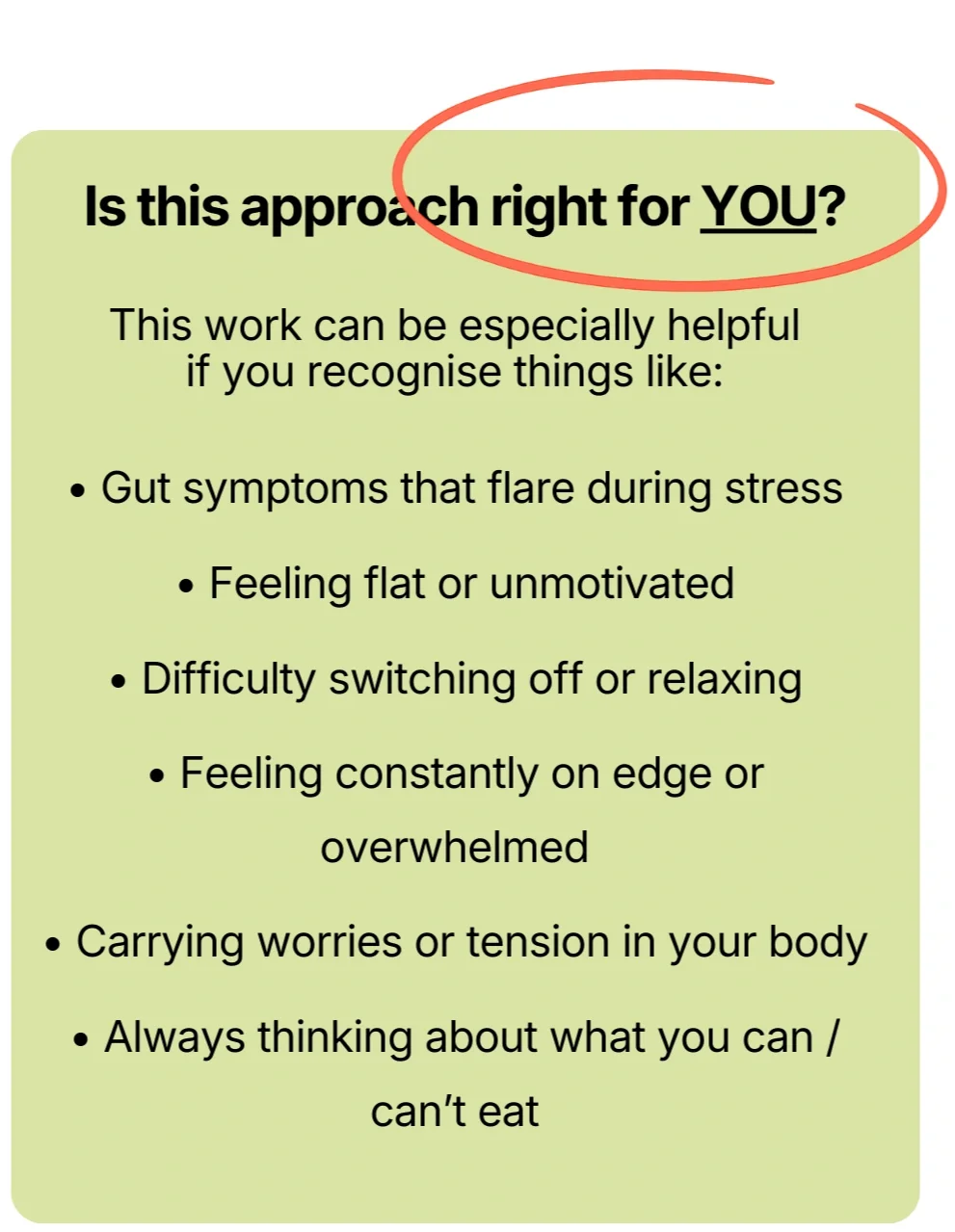
As a qualified digestive health nutritionist, I use evidence-based strategies and functional testing when appropriate to understand what is driving your symptoms. A good gut health specialist looks beyond a simple meal plan and takes time to understand your history, lifestyle, stress patterns and the gut brain connection. This personalised and ongoing support is what makes long-term improvement possible.
Q3: Why work with a nutritionist specialising in gut health compared to, or alongside, my GP?
A: Your GP plays an important role, especially in ruling out serious conditions. However, GP appointments are often brief and focused on symptom management. A gut health nutritionist has the time to look deeper into your history, lifestyle, diet and stress patterns to understand what is driving your digestive symptoms.
While a GP may focus on diagnosis or medication, a gut health specialist provides personalised and holistic support that addresses underlying causes. The two approaches work well together. Medical care ensures safety, while nutrition therapy provides the depth needed for lasting digestive change.
Q4: Can I manage bloating or reflux on my own, or do I need a gut health nutritionist?
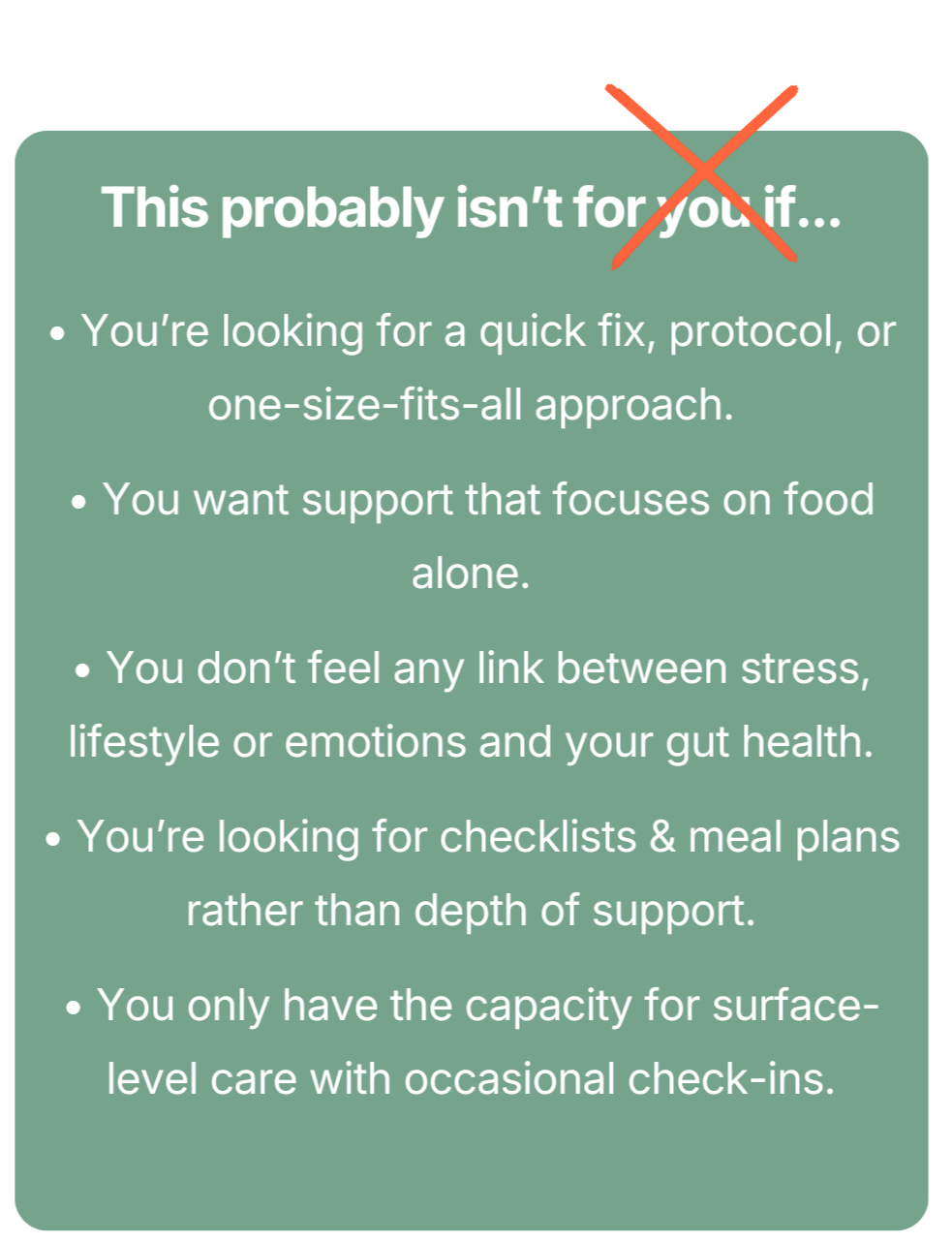
A: Many people try to manage gut symptoms on their own by changing their diet or using supplements, but results are often short-lived or inconsistent. A gut health nutritionist brings expertise in identifying root causes, using science-based strategies and applying functional testing when helpful.
They also provide a personalised plan and ongoing support that adapts to your lifestyle, stress patterns and changing symptoms. This type of guidance addresses diet, microbiome balance, the gut brain connection and nervous system support. These are key factors in achieving long-term digestive relief.
Q5: Do I need to have in-person consultations?
A: Not at all. Most clients work with me online and find it easier to stay consistent that way. As an online gut health nutritionist, I offer the same depth of support that you would receive in person.
Whether you are looking for a London gut health nutritionist or prefer to work from home, the process is the same. We explore your diet, microbiome and nervous system to understand what is driving your symptoms. You receive a personalised plan, targeted nutrition for gut repair and ongoing guidance, all with the convenience and comfort of home.